Post-COVID-19 Physicals For Public Safety Professionals

As COVID-19 continues to rage across our country, public safety professionals continue to face additional challenges compared to most other occupations. The issue that leaders in public safety seem to be grappling with the most revolves around how does the virus impact firefighters and law enforcement officers and their ability to safely return to work after getting COVID-19. At Front Line, the question we have been trying to answer is how can we help the individual firefighter or law enforcement officer get the analysis and have the confidence that they are ready to safely return to work? Additionally, how do we advise our fire and police chiefs that their members returning after an infection do not pose a risk to themselves or their teammates?
It is important to note that there is extraordinarily little to no published data on return-to-work guidelines for public safety professionals. The most current literature, published by national organizations such as the American College of Cardiology, relates most closely to return-to-play guidelines for athletes. We view our public safety brethren as tactical athletes. As such, our decisions, rationale, and methodology derive from the sources we feel are most applicable to this population. However, we view all screenings and recommendations through the lens of operational suppression and the workers' compensation system. Returning to work as a public safety professional is a much different equation then simply returning to the field. The role of medical screening prior to returning to work is constantly evolving. Which is why our return-to-work evaluations had to evolve, too.
While the long-term complications of COVID-19 are still being uncovered, our current post-COVID-19 evaluation includes diagnostic imaging, cardiac and other biomarkers, as well as cardiopulmonary exercise testing (CPET). While cardiac magnetic resonance imaging (CMR) is the gold standard assessment of left ventricular/right ventricular structure and function as well as myocarditis/pericarditis, it also requires specialty trained radiologists, lengthy and invasive testing procedures (gadolinium administration), and significant cost — and it does not evaluate the real-time gas exchange critical to operational suppression. Therefore, the use of CPET is the most cost effective and detailed diagnostic tool we have that simulates operational suppression under maximal effort, requiring the use of a self-contained breathing apparatus (SCBA), making it our test of choice.
The goal of our post-COVID-19 physical evaluations is to identify public safety professionals who have findings suggestive of myocarditis/pericarditis and then refer them to a specialist for further evaluation if necessary. Based on the most current research, the issues of greatest occupational/tactical concern as it relates to COVID-19 and public safety professionals include:
- Myocarditis, pericarditis, right ventricular dysfunction in the absence of significant clinical symptoms
- Myocardial injury that may precipitate malignant ventricular arrhythmias
- Severe acute respiratory syndrome and pulmonary emboli
- Severe cases have shown biventricular heart failure, cardiogenic shock, and death
Additional issues that have significant occupational impact include:
- Reduced exercise tolerance
- Non-specific malaise
- Recurrent chest pain
- Difficulty breathing/syncope
- Palpitations
- Prolonged periods of recovery
- Anxiety
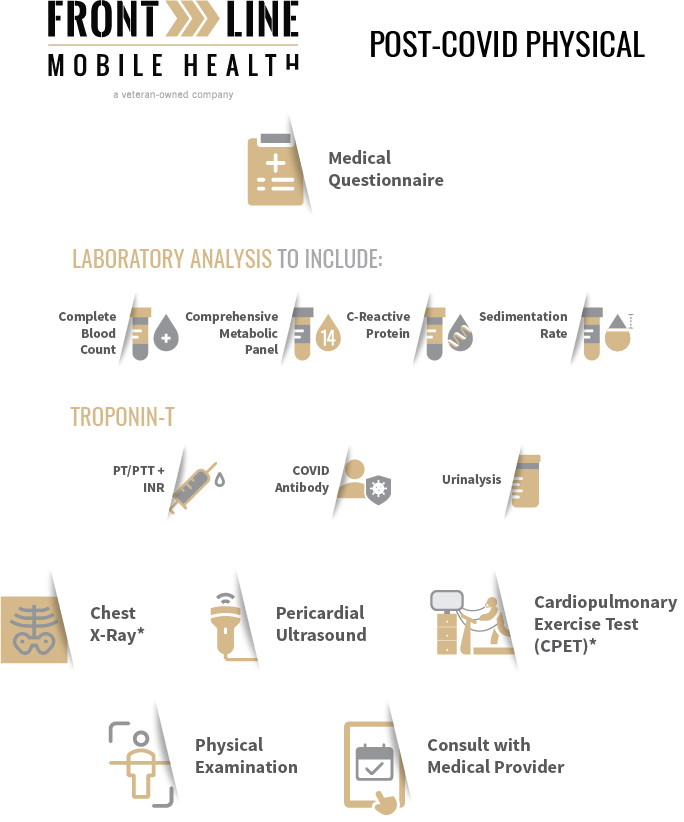
While the health and wellness of our clients is top priority, we also understand the organizational impact we can make. We believe in being good stewards of taxpayer dollars, and as part of that stewardship mindset, we have developed the following screening strategy to maximize available testing modalities. This allows us to provide detailed analysis to current patients, identify individuals who may benefit from further evaluation, and provide department leadership with the appropriate executive data to ensure safe return to work. This screening strategy includes:
- COVID-19 questionnaire
- Medical history
- Resting vital signs and body composition
- Two view plain film radiographs of the chest (with radiologist interpretation)
- Transthoracic ultrasound of the pericardium (with radiologist interpretation)
- Biomarkers (CBC, CRP, ESR, CK, Uric Acid, Troponin-T, Lactic Acid)
- COVID-19 antibody titers
- Pulmonary function testing
- Cardiopulmonary exercise testing (with cardiologist interpretation)
- Focused physical examination
- Medical consultation
As always, our team continues to stand on the front line of the most current research, recommendations, and developments. If you want to know more about our post-COVID-19 physical evaluations for a safe return-to-work program, please contact us. Like you, we are ready to serve.
Written by Alex Jesko, Exercise Physiologist